-
 Mail us
Mail ussupport@integrativebillingsolutions.com
-
 Toll Free
Toll Free(201) 257-9360
- Make Appointment
Phone
Location

Integrative Billing Solutions is a Medical Billing Company offering medical billing consulting services. Our professional billing consultants work side-by-side with healthcare providers to help them achieve billing success. We immerse ourselves in your practice to pinpoint opportunities for reducing denials and speeding up payments.
Our medical billing consulting group provides the strategic guidance and tactical support needed to optimize billing processes, technology, and staff skills. With our consultancy solutions, every practice is positioned to thrive through improved medical billing.
We provide comprehensive medical billing and revenue cycle management (RCM) services designed to optimize reimbursements and reduce administrative burden.
Our core services include:
Additional support services:
As a medical billing consulting company, we have subject-matter experts for every specialty’s billing and coding workflows. By leveraging efficient claim filing, precise coding, vigilant A/R follow-up, mastery of ICD-10 billing, and proper auditing – Integrative Billing Solutions medical billing audit consultants help healthcare providers receive every dollar they’ve earned when they’ve earned it.
We assist practices large and small in overcoming lost, delayed, or underpaid claims. Engage our medical billing and coding consultancy for the medical billing help your practice needs.


We strive to empower healthcare providers by simplifying the medical credentialing and enrollment services, enabling them to focus on their core mission of saving lives.
Integrative Billing Solutions's comprehensive medical credentialing services enable healthcare providers to simplify the provider enrollment and credentialing process, avoid claim delays, and save time and resources. With our centralized process and knowledgeable experts, providers can recognize revenue sooner and free themselves from the hassle of handling piles of printed documents and tiring follow-ups.

We assist healthcare providers in enrolling with Medicare and Medicaid.

Assist healthcare providers in navigating commercial insurance credentialing.

We streamline NPI registration for both individual providers (Type I) and organizations (Type II)

We do the registration of your Council for Affordable Quality Healthcare (CAQH) profile

We assist healthcare providers in obtaining and renewing state licenses

Our services cover the application and renewal processes for (DEA) certificates

We facilitate the revalidation and re-credentialing process for healthcare providers.

Our team provides expert support in contract negotiation with insurance payers.
Expand your patient reach and grow your practice with our seamless physician credentialing and contracting services. Our expert team streamlines the enrollment process, saving you time and hassle while maximizing your revenue potential.
Necessary documents vary for different insurance plans and types of physicians/practitioners. Here is a list of some basic documentation that is usually required.
Documents for individuals:
Documents needed for your legal entity:
Turnaround time varies between insurance carriers, so there is no one answer to this question. Major carriers generally take between 90-120 days to complete the process. Smaller carriers and insurance plans may take longer.
Upon submitting a participation request to a commercial carrier, providers will need to undergo two processes. The first of these is credentialing, where the carrier verifies all provided credentials and presents them to their committee for approval. Once providers are approved by the credentialing committee, they are then directed towards the contracting process wherein their participation is approved, and they are provided their effective date.
Commercial carriers do not allow for retroactive billing, meaning providers will only be compensated for claims submitted after they are listed as an “In-Network” provider in the carrier claims system. Out of network billing will result in much larger bills for patients and patients may be responsible for the entire bill on their own.
Applications of enrollment in Medicare typically take between 60-90 days to complete, though this does vary wildly between states. The effective date for Medicare is set as the date the application was received, allowing for providers to retroactively bill for any encounters that occurred between application and approval. There is also a 30-day grace period, enabling providers to bill for service provided up to 30 days prior to their effective date.
Turnaround time is longer for DMEPOS suppliers. In addition to the close scrutiny that every application is subjected, suppliers will also be required to participate in a site visit as part of the application process. The site inspector will be responsible for ensuring the office is located at the address included on the application, as well as hours of operation, where inventory is stored, and other important elements of being a DME supplier.
Sadly, Integrative Billing Solutions cannot make the process any quicker. Our contribution is efficiently and effectively managing the entire application process, beginning with initial credentialing applications and carrying through to follow-ups with carriers. Our experts are well versed in the entire process, saving time that might otherwise have been wasted by providers attempting to perform the process themselves and making mistakes along the way.
Yes, it is necessary for providers to have a place of service before they begin the medical credentialing and contracting process. A home address cannot be used as a clinic address, wither permanently or temporarily. A home address can, however, be used as an address for billing or correspondence, but only if a physical address for the practice is also provided. In the event that the office space is still under construction, the address can still be used. The application can be sent up to 30 days prior to the location actually opening up to patients, and most commercial carriers also offer the same guideline.
Revalidation of Medicare enrollment is required every 5 years but DMEPOS suppliers revalidate every 3 years. Individual providers can either complete the CMS855I paper application or use PECOS to complete the revalidation online. For groups or suppliers, the CMS855B application must be completed. If an Electronic Funds Transfer was not previously set up for the group record, one will need to be created for the revalidation process.
Providers must respond to their Medicare carrier within 60 days of receiving their revalidation letter. It is important to respond promptly, otherwise billing privileges will be terminated.
The CMS855I is used for individual provider enrollment in Medicare. It can be used by both physicians and non-physicians. Other necessary documentation will very between provider types.
Providers may also need to submit the CMS460 form to elect for participation in Medicare, without this form provider may be enrolled as non-participating providers. Non-participating providers will receive less reimbursement from Medicare, though they are also entitled to pursue more reimbursement directly from patients; up to 115% of the Medicare rate.
For providers enrolling under an existing group practice, the CMS855R form will need to be submitted. This form reassigns the provider’s financial payments to the business ender which their services are performed.
The CMS588 will be needed for both individual and group practices, in order to setup Electronic Funds Transfer to receive Medicare payments. Medicare does not issue paper checks; reimbursement is only dispensed via ETF.
The CP575 is the confirmation letter sent to providers by the IRS when they receive an Employer Identification Number, or Tax ID number, for a business. This letter must also be included in the application for Medicare enrollment as proof of the legal name of the business. In case the original is unavailable, a replacement letter 147C can be requested as verification of the EIN. These two documents are the only proof of EIN accepted by Medicare.

Integrative Billing Solutions offers a comprehensive range of Account Receivables management services, recovering outstanding revenue from old AR accounts that are aging more than 120 days. Our system has been proven to be highly effective at increasing recovery, even from accounts that were thought to be lost cause
Unlike most medical billing companies, who only offer AR recovery solutions as part of a revenue cycle management package, Integrative Billing Solutions offers AR medical billing recovery services as a standalone option. We don’t believe in a one-size-fits-all approach to healthcare receivable recovery solutions and want to meet the unique needs of your business.

Our Team efficiency allows you to reduce medical account receivables

We prioritize claims to ensure that none expire unnecessarily

we assign a dedicated team to focus on investigating every claim in your AR records.

We charge fees only as a small percentage of the amount recovered.

Our team has been able to consistently recover over 90% of claims.

Errors or omissions are easily correctable by our medical recovery services
Our dedicated taskforce doesn’t let a single claim be rejected, denied or underpaid due to lack of follow-up. After the appropriate corrections or clarifications are made, we appeal each of those claims so the insurance or government payer will reconsider the payment. We also monitor your claim denials and rejections, so we can identify any recurring causes and eliminate them permanently from your revenue cycle management system.
If the AR team finds that the outstanding balance should be paid by the patient, we generate a report that is easy for them to understand and send it to them. If you would like us to also handle the direct interactions with your patients, we will do that too. We aren’t a collection agency, so you don’t have to worry about sending the wrong message to your patients. We’ve found patients are much more likely to pay their bills if they understand the charges and agree with the amount due, so we help make everything clear and easy to understand. We’ll even take their phone calls and answer questions if you would like us to.

Our Virtual Assistant (VA) & Front Desk Support service is designed to handle your day-to-day administrative and patient-facing tasks with professionalism, accuracy, and consistency. We act as an extension of your practice, ensuring smooth operations, improved patient satisfaction, and reduced overhead costs—so you can focus on patient care.
Our Virtual Assistant & Front Desk Support services are tailored to meet the unique needs of your practice. Whether you need part-time help or full-time coverage, we provide dependable support that saves time, lowers operational costs, and enhances your patients’ experience.
Let us handle the front desk—so you can focus on delivering quality care.
While everything has evolved and moved on to digital platforms, why shouldn’t the doctor’s office do the same? A virtual medical assistant is a virtual assistant who works from home and manages and assists the physician in all the healthcare checkups and procedures online. They manage their appointments, maintain the calendar, and communicate on behalf of the practice. While they work from home, they save money on commutes and other things. The practice saves money on hiring an on-site medical assistant who would charge more for the job. Many companies provide such medical virtual assistant services, and you pay for them as per your package.
Virtual medical assistants frequently discover that they can use their skill set to earn money from any location with an internet connection, all while maintaining a healthy work-life balance. Often, all it takes to become a good virtual assistant is learning how to utilize applications that you may already be familiar with rather than a college degree.
As businesses become more comfortable with remote work, distributed teams, and outsourcing in general, the demand for virtual assistants has skyrocketed.
Greet patients online and address any initial inquiries or concerns. Update and maintain accurate patient records, ensuring data integrity and confidentiality. Schedule patient appointments and manage the appointment calendar efficiently. Handle incoming and outgoing emails and phone calls professionally and on time.

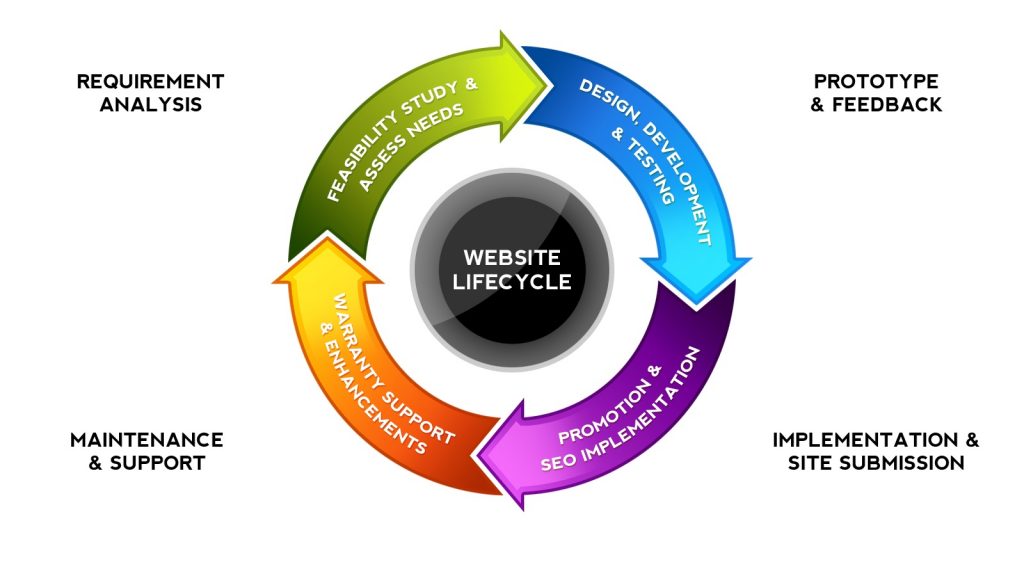
We constantly test, update, and refine our development processes. Our developers are also committed to ongoing learning so that your project can benefit from recent innovations and technologies. All of this allows us to provide you with a streamlined experience, from initial brainstorming to the implementation and maintenance of your solution. Your product will have the following:

Features tailored precisely to your requirements

Visually appealing and easy-to-navigate UI/UX design

Scalability and industry-standard security from the get-go

Responsive design for all devices

Ongoing maintenance and support
In the modern digital environment, a website is the face of any business. A well-structured website with user-friendly design adds value to a business, increases footfalls and leads to business growth and development. It is therefore critical that a lot of focus be given to this aspect. It is all the more important today as consumers prefer to check websites, compare prices offered by different companies before settling on a purchase, regardless of the products or services opted for.